After working in Africa for over 20 years, you think you’ve seen and/or experienced almost everything. But there are always new situations that, if you saw them on TV, you would wonder whether the scriptwriter had been drinking too much or smoking something illegal while working.
This assignment was a classic example of how life writes the best stories – without any help.
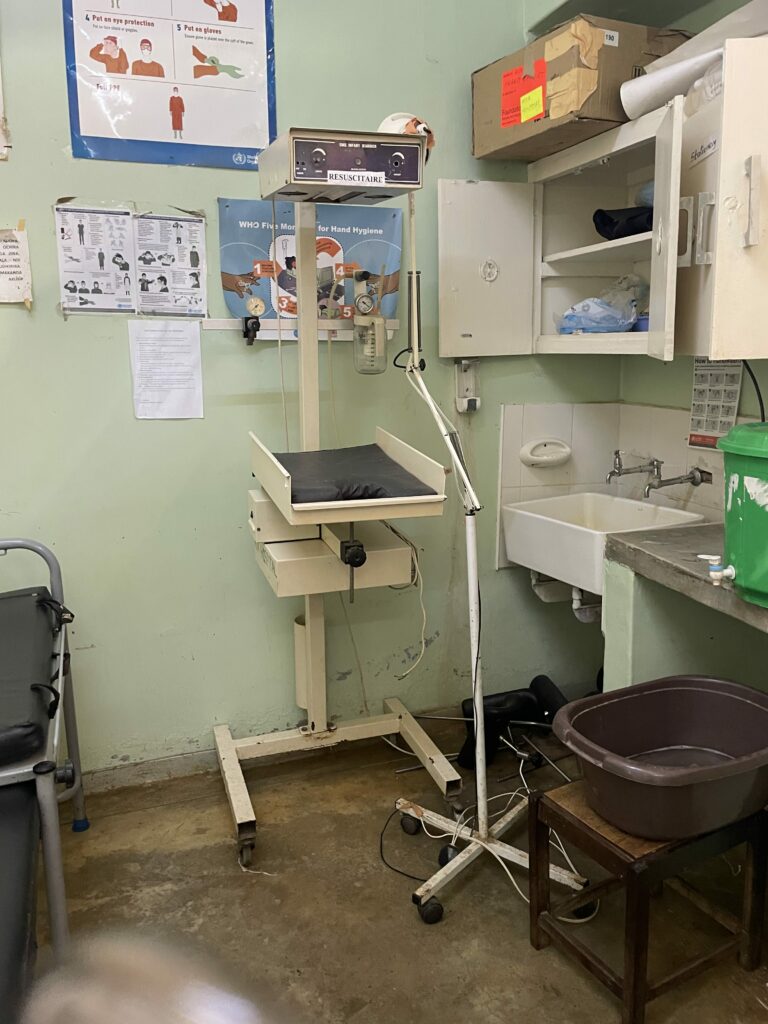
The ArtClinic team has now been to Mua, a small town about 3.5 hours’ drive north-east of Lilongwe, for the second time. The approximately 60-bed hospital is run by the diocese in Dezda and currently employs one doctor and 5-6 so-called “Clinical Officers” from various disciplines. A “clinical officer” is roughly equivalent to a German “physician assistant”, but has more powers. For example, the gynecological CO performs caesarean sections and hysterectomies independently.
The journey to Mua takes around 25 hours from door to door. When you arrive, you feel like a fish stick that is no longer quite fresh and is looking forward to a shower rather than a frying pan. Then it doesn’t matter that there is only cold water and you have to move precisely from jet to jet under the shower head.
We arrived in Mua in the late afternoon, dusty, tired, but full of energy – it was time to get going. Not only had we arrived, but also a crowd of people who wanted to make sure they were really seen. However, there were significantly fewer patients than in the fall and when we asked how this was possible, we were told that the patients now had to pay 25,000 kvashas (about €12.50) for the operation. 12.50 is a lot of money for an average monthly income of around €40. This regulation was decided without our knowledge and was abolished with immediate effect after several discussions. Our Malawian support Geoffry was deployed as a very effective bush telegraph and the next morning the usual picture of many waiting patients presented itself. It was never really clear who was trying to enrich themselves.
We screened a total of almost 80 patients, 43 of whom were put on the surgery plan. A further 15 were placed on the waiting list. Unfortunately, some patients could not be helped because they had illnesses that we could not treat, were very small or very pregnant. In the autumn, we started working with Dr. Leonard Banza, a Malawian doctor who works in Lilongwe and travels frequently to rural areas. He sent us a list of 13 children under the age of 10 who had suffered terrible scar contractures on their limbs after exposure to fire, hot water or other liquids. Unfortunately, only 10 of them turned up, the other three hadn’t come because they thought they had to pay and so had gone home. We were boiling with rage, so much so that if the person who had unauthorized the op fee had come around the corner, he probably would have caught a burn from the angry heated looks we gave him.
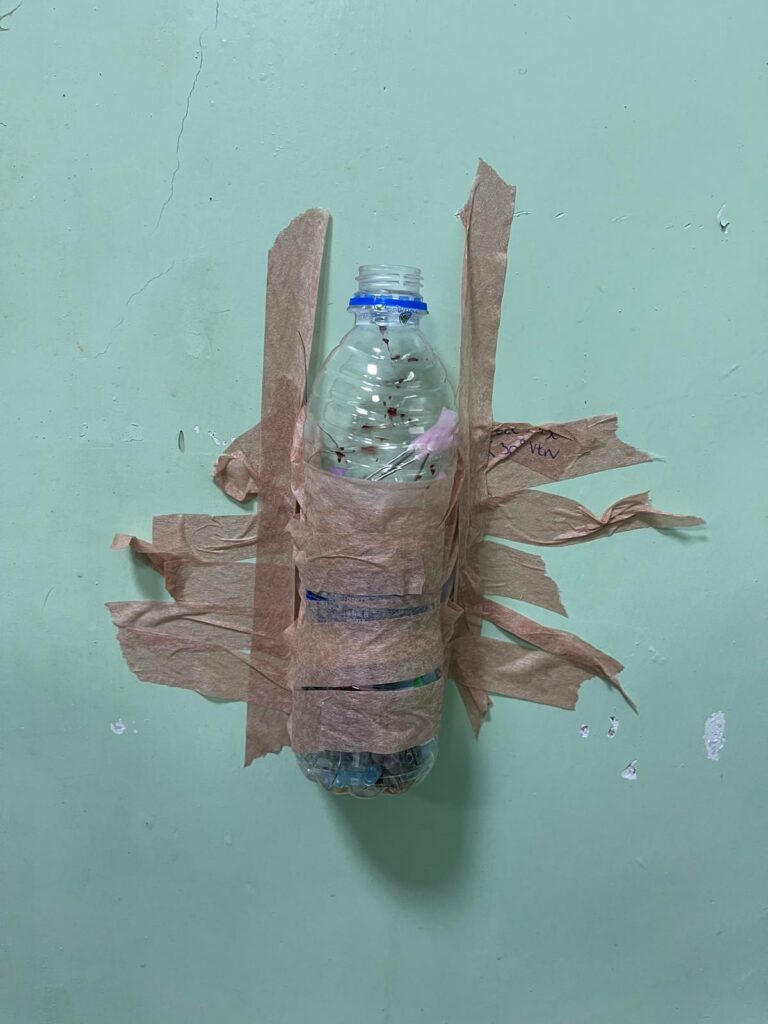
Our anesthetists had planned to administer the anesthesia Malawi-style, i.e. with Propofol, Ketanest and Halothane. That went well until the halothane ran out and we couldn’t get any more in the entire Dezda region. A few operations then had to be grudgingly performed under local anesthesia and two more under spinal anesthesia. Sister Dr. Eva, a Malawian nun, who is also the medical director, was able to find a bottle of Halothane through abstruse means, which I then paid dearly for in a corner of a parking lot in Lilongwe (3.5 hours’ drive) from the trunk of a black Mazda with tinted windows. The money was taken by a guy with a gold chain around his neck that could have been used to anchor the Queen Elisabeth cruise ship. Sister Dr. Eva had told me the price I should pay, but I was not surprised when he demanded a much higher price. After pointing out that I had been quoted a much lower price by Sister Dr. Eva, he broke into a sunny smile and said “Aaah – Sister-discount!” Only real life writes stories like this…
We were able to operate on a total of 41 patients, 22 under general anesthesia and 19 under local anesthesia. We operated on 10 children with severe scar contractures, 6 of whom have been called in again for October because further operations need to follow. Skin defect coverings with skin grafts were performed on 12 patients, 15 patients were operated on for facial tumors (dermoid cysts, atheromas, neurofibromas, lipomas) and 19 other patients were treated for soft tissue changes on the hand, extremities or trunk.
Our “soft tissue tumor school”, in which Dr. Eva (general practitioner) and 5 clinical officers learned how to diagnose different soft tissue tumors and then operate on them “hands on” under supervision, was very popular. Sara, Alexa and Gie were also able to show the young colleagues how to perform “continuous suturing” with absorbable material, which means that patients no longer have to come back for stitches and can save money on another trip to the hospital.
As always, there are a few patients who are particularly memorable. For example, the 60-year-old woman from whom we removed a 3 kg lipoma from her back and who then beamingly announced that we didn’t need to tell her that everything had gone well because she could now lie on her back again for the first time in 30 years. Or the 9-year-old girl who had developed a severe submental contracture with a pronounced pull on her lower lip after a fire four years ago and was finally able to close her mouth again after the operation. The mother happily told us that the little girl could now drink again without water running out of her mouth.
It is a gift that we can help those who really need help. There are always moments when I don’t know where to find the strength to fight against incomprehensible rules, customs regulations, licensing, bureaucracy and the boundless arrogance of some authorities, but at this point I always remember my father’s saying: “For the big picture, our work is a teaspoon in the ocean; for the individual, it’s the whole ocean.
The operation could never have taken place without the donors from Interplast. Thank you, Mrs. Völpel and Dr. Borsche, for allowing us to participate. Thanks also to the Klindwort pharmacy in Bad Schwartau with Ms. Schubert and Ms. Lehmann, who collect medicines for us, and a big thank you to our families and friends who support us again and again. A very special thank you goes to Mrs. Vera Klischan, who actively supported us in the recovery room and kept us happy with her wonderful sense of humor. Together we were able to make the world a little bit better.
The team: Dr. Bertil Andersson, Cäcilie Jansson, Sara Lindahl, Alexa Meyer Vandehult, Dr. Henrik Sundemann, Dr. Gie Vandehult
For the ArtClinic team: Dr. Gie Vandehult